discussion
Moreover, as noted above, all of our patients had AMI exactly 1 year ago and did not have any MACCE within 1 year of onset. Therefore, even though our participants did not strictly meet the general definition of “stable post-MI populations” (i.e., the time between patients’ last MI or coronary intervention and inclusion was more than 1 year), our populations did are MI patients who were relatively stable. Comparing our results to the studies where the study populations was stable post-MI patients, CORONO study conducted by Delsart P et al. showed that the rate of all-cause death for their stable CAD patients without coronary vascular intervention history was around 5.5% at 1 year,20 which was higher than the corresponding rate in our 18-month DAPT group (3.7%) and similar to the rate in our 12-month DAPT group (5.9%). The baseline rate of DAPT use for their non-coronary vascular intervention patients was 20%, and angiotensin system antagonists, beta-blockers and statins were widely prescribed in these patients. According to the results, continuous at least 18-month DAPT is likely to reduce all-cause death rate for stable MI patients without revascularization because our patients had a shorter period of time since their last MI onset and should have been at a relatively higher risk of death compared to the stable patients with a history of MI >1 year,5,21 but as far as the current results are concerned, our patients who consistently used DAPT (18-month DAPT group) had a lower all-cause death rate, indicating a potential benefit of prolonged DAPT. In addition, PEGASUS-TIMI 54 trial,22 a landmark double-blind randomized controlled trial (RCT) for the patients who had had a MI 1 to 3 years, demonstrated that the rate of composite endpoints of cardiovascular death, MI, or stroke in DAPT group was around 3.5%, while the rate of composite endpoints was 4.5% among placebo aspirin group at 18-months. Additionally, the DAPT group reduced the risk of composite outcomes by 15%~16% at 3 years, compared with the reference group. Although the incidence of endpoints in PEGASUS-TIMI 54 trial was slightly higher than our results at 18 months (MACCE: 18-month DAPT group: 1.9%, 12-month group: 4.3%), their study, similar to our findings, supported that the continuous DAPT reduced the risk of ischemic events. Furthermore, the analysis of the stable population subgroup of the CHARISMA trial (40.6% participants of the subgroup had prior MI) showed that the rate of composite outcomes of cardiovascular death, MI, or stroke at 18 months was 4.5% in DAPT group and 6% in aspirin placebo group, and appeared to derive a benefit of 17% deduction in the risk of cardiovascular death, MI, or stroke from DAPT with clopidogrel plus aspirin during the 28-month follow-up.23 Therefore, this study also indicated that continuous DAPT appeared to have a significant benefit for stable MI population, which was consistent with our results. Overall, the previous published studies on stable CAD directly included patients with a history of MI, and their MI histories span a wide range of time, from 1 year to around 30 years, and treatments patients taken were different, such as PCI, coronary-artery-bypass-grafting (CABG) or medical management. Thus, in fact, their populations were very heterogeneous which means the overall effect derived from the studies is a relatively rough average, overestimating the effect for some patients and underestimating the effect for another participants. On the contrary, our study was a continuation of patients with AMI (exactly 1 year ago), and in our population, undergoing primary, elective interventions, and thrombolysis were all excluded, which means our subjects were a determined MI population, with the use of medication exclusively. Therefore, our findings are relatively more precise due to the clarity of our target population. In addition, we used all-cause death rather than cardiovascular death as the endpoint because our death records were mostly from death registration. In this real-world observational cohort, all-cause death record has relatively higher accuracy and data completeness. There were some other studies of DAPT using all-cause death as their study outcome as well.18,24 Thus, in relation to previous studies, our study mainly focused on all-cause death and drew a conclusion for this “hard endpoint” in MI patients.
There are some limitations in our study. Almost all of the P2Y12 inhibitors used in our study were clopidogrel, thus the results may not reflect influence of other P2Y12 inhibitor drugs. The cause of death could not be determined as it was mostly from death registration. Although we have adjusted several potential confounders between two treatment groups, there are likely to be some other unknown variables resulting in selection bias. The records of important post-discharge events were from the descriptions of patients and their relatives, which may cause recall bias. In addition, a large number of patients in China did not use DAPT to 1 year, not only leading to small sample size of our study, but also probably resulting in the occurrence tendency test unreliable.
In terms of bleeding risk for prolonged DAPT, unlike the results of other studies which found that prolonged DAPT was associated with increased major bleeding events, our study showed that prolonged DAPT did not significantly increase the risk of bleeding relative to long-term DAPT in our participants. This inconsistency may be related to the following reasons. It is known that several factors such as advanced age (> 65 years), low body weight, diabetes, or chronic kidney disease may increase bleeding risk.25 However, as shown in our baseline analysis, only a minority of participants in our study had risk factors noted above and these variables were distributed without significant difference between our two treatment groups, which may account for the inconsistent findings regarding bleeding risk. Furthermore, we have excluded the patients who had major bleeding events within 12 months when we included the participants, which also reduced the bleeding risk in our study population to some extent. In fact, the incidence of bleeding events was very low in both of our 2 treatment groups, with 3 (0.3%) and 1 (0.2%) case for long-term DAPT group and prolonged DAPT group, respectively, at 24 months. Therefore, prolonged DAPT may not significantly increase bleeding events in the MI patients with a relatively low bleeding risk. Additionally, a study carried out by Costa F et al. found that the bleeding risk was increased by long-term DAPT (12 or 24 months) only in the high-bleeding-risk patients, which also provided support to our results.26
Furthermore, for the AMI patients without revascularization, medication is particularly critical to their prognosis. Therefore, we included medication adherence of several important drugs, including statin, β Blocker, and ACEI/ARB, in our fully-adjusted multivariate model. As shown in results, in our study, there was no significant reduction in all-cause death risk for 18-month DAPT group relative to 12-month DAPT group at 24 months, with an adjusted HR equal to 0.698 (95% CI, 0.416-1.172). It may be related to some potential reasons. First, at 18 months follow-up, DAPT use was significantly better in 18-month DAPT group than in 12-month DAPT group (i.e., the rate of aspirin and P2Y12 inhibitor usage was both 100% for patients in 18-month DAPT group, while the rate of P2Y12 inhibitor usage in 12-month DAPT group was only 1.5%). However, at 24 months, the actual use of DAPT was only 194 persons (37.1%) in 18-month DAPT group. Thus, in fact, the majority of patients in 18-month DAPT group strictly used DAPT for only 18 months, and this result indicated that discontinuation seemly means loss of cardiovascular protection. Furthermore, several studies suggested that discontinuing aspirin after DAPT and continuing the P2Y12 inhibitor may be associated with good prognosis in the patients, indicating the importance of P2Y12 inhibitor use.27-30 However, in our study, the actual use of P2Y12 inhibitor in 18-month DAPT group was relatively low at 24 months. This may also explain why the result of HR for all-cause death was statistically significant at 18 months but not at 24 months. Moreover, for further exploring potential benefit of 24-month DAPT, we carried out the subgroup analysis (shown in Supplementary Table 1) and found that the 24-month cumulative event rate of all-cause death did occur significantly less frequently in the subgroup of 24-month DAPT (i.e., strictly continuing DAPT at least 24 months) than in the subgroup of 18 months≤DAPT<24 months (i.e., probably discontinuing after 18 months), which complemented and explained the results mentioned before. Therefore, our results suggested that discontinuation of DAPT, especially discontinuation of P2Y12 inhibitor, probably mean a loss of protective effect in MI patients without revascularization. Second, the number of MI patients without revascularization in clinical study is limited, and in developing countries, such as China, even fewer patients follow medical advice and are on long-term DAPT (at least 12 months), resulting in our relatively small sample size. Small sample size may lead to a failure to test for positive treatment effects. Therefore, it is probably appropriate to describe the 24-month result as inconclusive rather than negative. In this case, the sample size required to test effects of the treatment may be met by including additional high-risk populations in the future.31
In PCI era, although MI patients without revascularization are less probable to receive evidence-based medications, this actually occurs more often when they are cared for by non-cardiologists, and it is one of reasons they became the target population of our study. 15,16 There have been some DAPT-related studies focusing on MI patients without revascularization. For instance, the CURE trial conducted by Yusuf S et al, a study that more than 60% of its patients with ACS did not undergo coronary revascularization, showed that 3~12 months DAPT led to a 20% relative risk reduction of the composite endpoints of cardiovascular death, MI or ischemic stroke, which suggested the necessity of DAPT for medically managed patients,17 as in our study. Moreover, another large retrospective cohort study also revealed the effectiveness of DAPT for this kind of population.18 The evidences thus far reveal that taking DAPT at least 12 months has a significant mortality deduction and a protective effect against ischemic complications in MI patients, regardless of the presence of ST elevation and whether reperfusion is undergone or not.19 Under this situation, our study of MI patients without revascularization adds to the research gap on whether there is any additional benefit to continuing DAPT after taking DAPT for a full 12 months in such patients, and concluded that continuing DAPT to at least 18 months is associated with a reduction in the risk of all-cause death compared with discontinuation of DAPT.
In this multicenter, prospective AMI patient registry, we included patients who did not receive revascularization after an AMI and remained free from any ischemic events, such as death, MI, stroke, or bleeding, within one year from the onset. Prolonged DAPT (18-month DAPT group) had a significantly lower cumulative all-cause death rate than 12-month DAPT use at 18 months. There was no significant increase in bleeding risk for the prolonged DAPT relative to the long-term DAPT.
Limitations
美国心律学会年会公布研究:短期喝大量西柚汁或可引发致命心律失常
在日前召开的美国心律学会(HRS)年会上,以色列研究者报告的一项研究显示,短时间内喝大量西柚汁可能会导致QT间期延长,女士和长QT综合征患者尤其风险高。这一研究结果同时发表在《心律》杂志上。QT间期延长表示心脏复极延迟,是心电异常的一种表现,通常与心律失常敏感性增高密切相关,严重时可出现尖端扭转型室性心动过速甚至猝死。Heart研究:心率每增加10 次/分,心血管死亡风险增加11%
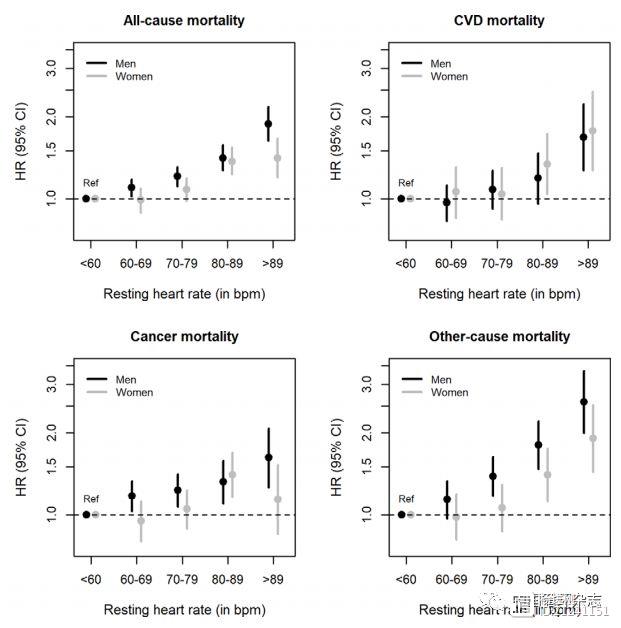
Heart上发表的一项研究显示,静息心率快及十年内静息心率增加则死亡风险高。研究发现,静息心率每增加10次/分,心血管疾病、癌症和其他原因死亡率分别增加11%、10%和20%。图1静息心率与全因死亡及某些原因死亡风险而且,在10年期间,与静息心率稳定者相比,静息心率增加>15次/分(男性)或>25次/分(女性)者死亡风险更高。 杨进刚阜外2023-08-17 11:56:470000
杨进刚阜外2023-08-17 11:56:470000《国际肥胖杂志》研究:晚上更易暴饮暴食,且压力促进食欲
《国际肥胖杂志》上的一份报告提示,晚上是吃得过多的高危时间,尤其是当你有压力时,很容易暴饮暴食。因为该研究发现,饥饿激素(即ghrelin)水平在晚上上升,饱腹激素(即激素肽YY,一种食欲抑制激素)水平在晚上下降。研究结果还表明,压力可能会在晚上增加更多的饥饿激素水平,而对于那些容易暴饮暴食的人来说,激素对食欲的影响可能更大。评估肥厚型心肌病手术效果有新超声指标!阜外医院王浩等研究
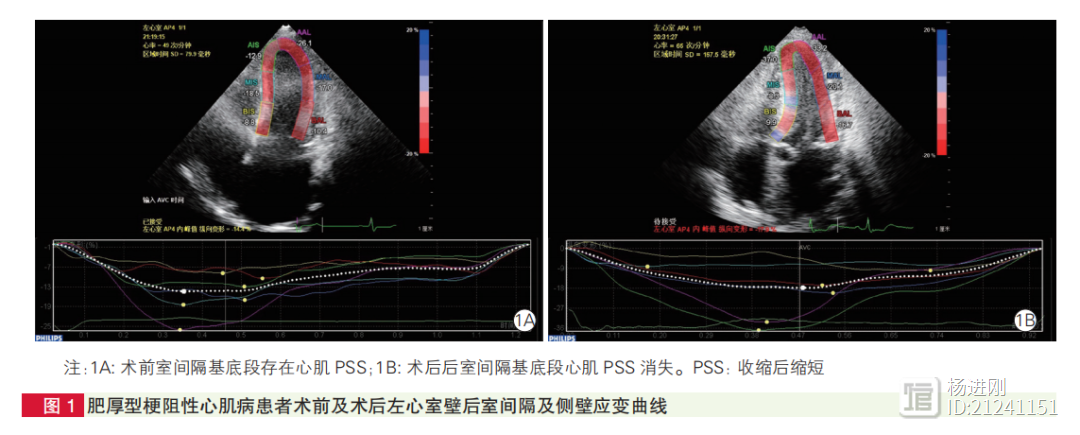
阜外医院王浩、段福建等通过应用超声心动图二维斑点追踪技术发现,肥厚型梗阻性心肌病患者接受扩大室间隔切除术后,左心室舒张功能有明显改善。研究者发现,与术前相比,肥厚型梗阻性心肌病患者术后左心室心肌收缩后缩短(PSS)发生率(6.27%vs.2.71%)以及平均心肌收缩后应变指数(PSI)[(3.68±2.79)%vs.(2.34±2.33)%]均显著降低,以基底段降低最为明显。 杨进刚阜外2023-09-10 17:45:220000
杨进刚阜外2023-09-10 17:45:220000术前左室重量指数有妙用!阜外医院孙寒松等主动脉瓣狭窄手术研究
阜外医院孙寒松、徐海涛等研究提示,主动脉瓣重度狭窄合并非对称性室间隔肥厚的患者行主动脉瓣置换术后左心房逆重构的最佳时期是术后3个月,而左心室逆重构的最佳时期是术后2年;术前更高的左心室重量指数容易导致术后残余左心室肥厚,与远期不良事件密切相关。

 正在请求数据,请稍候!
正在请求数据,请稍候!